This is an a online e log book to discuss our patient's de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centred online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment.
2nd December 2022
A 54 year old male came to OPD with chief complaints of -
bilateral pedal edema since 1 week
decreased urine output since 1 week
HISTORY OF PRESENTING ILLNESS
The patient was apparently alright 5 years back then one day he developed fever which was sudden in onset. The fever was associated with other symptoms such as vomitings, generalized edema and increased perspiration.
For this he consulted the local hospital where he was diagnosed to have hypertension and is on regular medication since then. He was adviced to come to our hospital for dialysis as he was found to have deranged kidney function.
He visited our hospital and was advised four sessions of dialysis despite which his condition didn't improve.
Subsequently, he was started on regular hemodialysis sessions about 2 sessions per week since the last 5 years.
H/o bilateral pedal edema since 1 week and decreased urine output since 1 week.
H/o pain in the left hip region and back which developed suddenly and he is unable to walk since 5 days.
PAST HISTORY
10 years back he was diagnosed to have hypothyroidism and started taking medication after 1 year.
He is a k/c/o HTN since 5 years
Not a k/c/o DM , TB, asthma, epilepsy, CAD, CVA
No h/o any previous surgeries
PERSONAL HISTORY
Daily routine before 5 years -
He used to work as a supervisor at a paint shop. His routine comprised of waking up at 6 am and leaving for work at 7 am. He used to be back by 7 pm and spend time with family. He used to have 3 meals per day. He used to smoke 1-2 beedi per day and consume 100ml of alcohol per day from past 20 years.
Daily routine since last 5 years -
He stopped going for work. Now he just stays at home and goes for his weekly dialysis sessions. He takes only 1 - 2 meals per day. He has given up on his addictions due to his condition.
There is significant weight loss from 80 to 45 kgs.
Appetite - decreased
Diet - vegetarian
Bowel & bladder habits - reduced
Sleep - inadequate
TREATMENT HISTORY
Since last 5 yrs on -
Tab Nicardia Retard 20mg
Tab Arkamin 100micrograms
Tab Lasix 40 mg
Tab Sobinid 500mg
Tab Calvic-D
Tab Calci
Since last 9 yrs on -
Tab Thyronorm 250 micrograms
Family History
Not Significant
GENERAL EXAMINATION
The patient is conscious, coherent, cooperative and well oriented to time, place and person.
He is thin built and poorly nourished.
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - absent
B/l pitting type of pedal edema seen
AV fistula on left arm since 3 years
Vitals on admission -
Temperature - 98 F
PR - 88 BPM
RR - 16 CPM
BP - 140 / 90 mm Hg
SYSTEMIC EXAMINATION
CVS - S1, S2 heard,no murmurs
Respiratory system - trachea is central, all quadrants of chest moving equally with respiration, normal vesicular breath sounds are heard, no adventitious sounds heard
CNS - no focal neurological deficits
Abdominal system -
On inspection - abdomen is flat & symmetrical
Umbilcus is central and inverted
No scars, sinuses & engorged veins seen.
All 9 regions of abdomen are equally moving with respiration
On palpation - abdomen is soft and non tender
On percussion - no shifting dullness, no fluid thrill
On auscultation - normal bowel sounds are heard
PROVISIONAL DIAGNOSIS
CKD on MHD
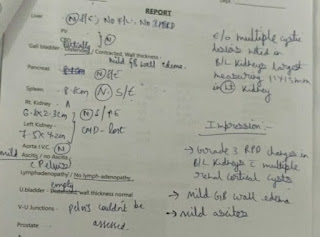
INVESTIGATIONS













Comments
Post a Comment