This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current based inputs
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
02-02-2022
A 80 year old male came to OPD with
CHEIF COMPLAINTS
Fever and chills since 11 days
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 11 days back since then he had fever which is insidious in onset, intermittent , high grade, with evening rise of temperature and associated with chills and rigors . Patient looks extremely lethargic, generalized weakness (patient is not able to carry out his daily routine and not able to sit or walk without attenders support, previously used to be active) and fever subsided on taking medication (paracetamol).
He has difficult while swallowing solid foods, able to drink liquids without any difficulty.
He has burning micturation since 1 week.
6 days ago they went to a local doctor where urine examination was done and said there is pus in the urine and treated him with antipyeretics and antibiotics.
He also has increased frequency of micturation and has dribbling of urine on straining and postvoidal residue since 6 days.
He also complains of being thirsty and feels dryness of tongue in spite of drinking water.
History of constipation since 5 days and he passed stool day before night after enema.
There is history of weight loss as noted by attenders.
Patient also complains of bilateral knee pain since 5 years and history of knee locking (suggestive of osteoarthritis).
No history of cough, body pains, shortness of breath, vomiting, diarrhea, shortness of breath.
PAST HISTORY:
No history of similar complaints in th past.
He is a known case of Hypertension and Diabetes since 5years and is on atenolol 50mg, Metformin 500mg and glipizide 5mg.
He is not a known case of asthma, epilepsy,CAD.
History of surgery done for benign prostatic hyperplasia (BPH).
PERSONAL HISTORY:
Daily routine:
He wakes up at 5am in the morning and gets freshened up and goes to get milk.He then drinks tea at 7am in the morning.Then he does few household chores like boiling water, cleaning the house.
Then at 9am he eats breakfast.
Then he takes rest for sometime and goes to a forest to get sticks and tie them together and make broomsticks.
Then at 2pm he eats his lunch and takes rest for sometime and goes out for a walk and then have dinner at 8pm.
He goes to bed by 9pm.
Diet-mixed
Appetite-decreased
Sleep adequate
Bladder movements-increased frequency.
Bowel movements- constipation since 6 days.
He drinks alcohol occasionally (90ml) and smokes daily 2to 3 beedi per day.
FAMILY HISTORY:
His 1st son died due to heart attack.
And his 2nd son died for liver failure secondary to shock
GENERAL EXAMINATION:
Patient is conscious non coherant cooperative
Moderately built and poorly nourished.
No pallor
Icterus is present
No cyanosis
No clubbing
No lymphadenopathy
No edema
Bilateral knee joint swelling(with flexion deformity)
VITALS:
BP: 130/80 mmHg
PR: 74 bpm
Temp : 98.6F
GRBS : 170mg/dl
SYSTEMIC EXAMINATION:
CENTRAL NERVOUS SYSTEM:
Conscious and non coherant
HIGHER MENTAL Functions Intact.
MMSE 24/30
CRANIAL NERVE EXAMINATION:
1st : Normal
2nd : visual acuity is normal
3rd,4th,6th : pupillary reflexes present
EOM full range of motion present
5th : sensory intact
motor intact
7th : normal
8th : No abnormality noted.
9th,10th,11th,12th : normal.
MOTOR EXAMINATION:
SUPERFICIAL REFLEXES:
CORNEAL present
CONJUNCTIVAL present
DEEP TENDON REFLEXES:
Right Left
UL LL UL LL
BULK: Normal Normal Normal Normal
TONE : Normal Normal Normal normal
POWER : 4/5 4/5 4/5 4/5
DEEP TENDON REFLEXES:
Right left
BICEPS. 1 1
TRICEPS 2 2
SUPINATOR 1 2
KNEE 2 1
ANKLE 1 2
https://youtube.com/shorts/L9VKzyXRt_w?feature=share
https://youtube.com/shorts/3R5VfOPGimY?feature=share
https://youtube.com/shorts/MWi6csdneKI?feature=share
SENSORY EXAMINATION:
SPINOTHALAMIC SENSATION:
Crude touch Present
Pain Present
Temperature Present
DORSAL COLUMN SENSATION:
Fine touch Present
Vibration Present
Proprioception Present
CORTICAL SENSATION:
Two point discrimination Present
Tactile localisation Present
CEREBELLAR EXAMINATION:
Finger nose test able to perform
Heel knee test able to perform
https://youtu.be/6IUtiGy19K0
Dysdiadochokinesia Absent
Speech Normal
Rhombergs test Absent
SIGNS OF MENINGEAL IRRITATION:
Kernig's sign, brudzinski sign, neck rigidity
absent
RESPIRATORY SYSTEM:Bilateral air entry present,vesicular breath sounds heard, no adventitious sounds heard.
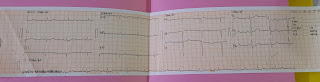
CARDIOVASCULAR SYSTEM:
S1 ans S2 geart sounds heard,no murmurs heard
ABDOMINAL EXAMINATION:
Soft and non tender,No organomegaly
PROVISIONAL DIAGNOSIS
UROSEPSIS(CUE -30-40pus cells,alb+)
With AKI(creat 1.7) - Resolved
Dyselectrolytemia (hypotonic hyponatremia improving with 0.9%NS Na 123 at presentation improved to 128,Hypokalemia 2.7 at presentation -after correction 2.9)
Acute liver injury
INVESTIGATIONS:
On 26-11-2022 :
On 27-11-2022
On 28-11-2022
On 29-11-2022
On 30-11-2022
1-12-2022
Culture
2D echo
USG
2-12-2022
3-12-2022
TREATMENT:
Inj Pentaz 4.5 gm IV stat
Inj KCL 2 amps in 500 ml NS
Tab doxy 100 mg/po/bd
Tab pan 40 mg/po/bd
Inj optineuron 1 amp in 100m NS
Lactulose

























































Comments
Post a Comment